Flu & Influenza
The history of the flu dates to as far as humankind. Familiar symptoms of the flu were first recorded around 400BC by Hippocrates, a Turkish seasonal winter to spring respiratory ailment that resulted in coughs, fevers, sore throats. Although these records illustrate similar symptoms, we will never be fully certain if this was influenza. The common cold and flu are caused in varying severity by about 200 different viral infections.
The term influenza originates from Italy in the 1400s; this was after the ‘Influence of the Stars’ epidemic raged across Europe, Asia and Africa. Over 31 potential outbreaks were recorded between 1404 – 1900, resulting in thousands of deaths.
Discovering the Flu Virus
Our history of viruses started in the 1880s, when scientists discovered something in fluids obtained from unwell patients that was much smaller than bacteria could also spread disease. Many people believed it was the fluid itself making people sick and it wasn’t until the 1930s when higher quality microscopes were developed, that we could see it was microscopic viruses spreading the disease.
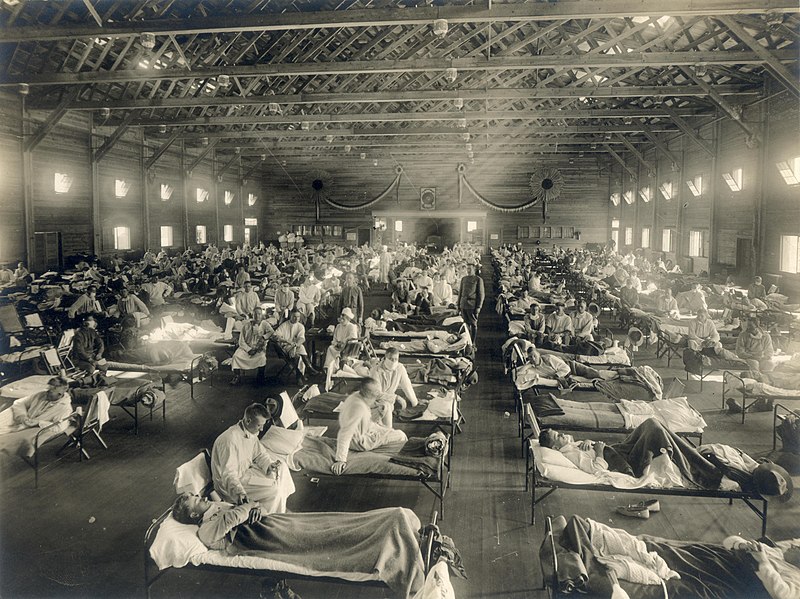
The First ‘official’ Recorded Flu Pandemic: The Spanish Flu
1918 dated the first official recording of an influenza pandemic, called the Spanish flu, that is estimated to have infected up to 30% of the global population, killing over 40 million people. It was only much later we recognised that the Spanish flu was an influenza pandemic. Frozen flesh samples analysed much later have shown us that it was a Type A H1N1 virus.
Over the following century, while influenza continually circulates the globe seasonally, there have only been four major pandemics:
- 1918 – The Spanish Flu
- 1958 – The Hongkong pandemic
- 1968 – The Asian flu pandemic
- 2009 – The Swine flu pandemic
Flu Strains: Why were these flu seasons so different?
Well other than a higher number of people being infected and a higher mortality rate, they also happened following the identification of a new strain of the virus. When new strains of virus emerge (which we have no immune memory to) they can spread like wildfire and cause more severe illnesses. Influenza is not just limited to certain areas, however, studies found that it is more prominent in the east of the world. Deadly outbreaks of influenza are almost always associated with strains that leap the species barrier and come from animals.
While we do know that a crossover of an avian H1N1 stain caused the 1918 Spanish flu, we don’t know if other H1N1 strains existed in humans before this, but we do know that the H2N2 and H3N2 strains emerged and caused the 1958 and 1968 pandemics respectively.
Flu Vaccines & New Strains
Thankfully we have effective vaccines to protect the most vulnerable from the potentially life threatening effects of influenza. The use of vaccines has also helped notify us when new strains of disease emerge. Quite often the emergence of the new strain will make the vaccine ineffective, alerting healthcare authorities and scientists to potentially dangerous new effects.
There are 4 subtypes of influenza: A, B, C and D
Only types A and B infect humans, but the symptoms of type B are less severe. Our seasonal vaccine protects us against 4 strains every year (two type B strains and two type A strains). Vaccines are selected based on what strains are circulating the most.
Covid-19 & Vaccines
In the aim of getting new traffic to this, we want to talk about covid. In this paragraph talk about how coronavirus differs from the flu, the main differences and similarities.
As the COVID-19 pandemic has taught us, we must remain vigilant to new strains emerging, but due to improved access to healthcare and good hygiene standards in the late 20th century and 21st century, death tolls of influenza pandemics have not been as severe.