All you need to know about informed consent in clinical trials
Clinical trials cannot be conducted without the participation of volunteers, and their informed consent is the foundation of ethical research.
Informed consent is more than just a formality; it is a continuous dialogue between the research team and the participants. It involves educating potential participants about the study clearly and comprehensively, answering their questions, and addressing any concerns.
By understanding and agreeing to the trial conditions, participants contribute to the advancement of medical knowledge while being safeguarded against potential risks.
- What is informed consent?
- What is informed consent in clinical trials?
- Why is informed consent important?
- What are the 4 principles of informed consent?
- When is informed consent obtained during a clinical trial?
- How is informed consent obtained for a clinical trial?
- What next?
Use the links above to skip ahead to the questions you’re most interested in.
What is informed consent?
Informed consent is one of the founding principles of research ethics. It’s the process in which patients are given information, including possible risks and benefits, about a medical procedure or treatment, clinical trial, or genetic testing.
Every patient has the right to ask questions and get information before procedures, treatments, or trials. Patients can then decide if they want to be treated, tested, or take part in the trial.
What is informed consent in clinical trials?
Informed consent in clinical trials includes the volunteer making an informed decision about whether to participate or not in a clinical trial. Participants will need to be informed about:
- what will be done to them,
- how the protocol (plan of research) works,
- what risks or discomforts they may experience,
- participation being a voluntary decision on their part.
This information is provided to potential participants through the informed consent process.
What information must be given to each potential volunteer?
A team member will meet with the participant to explain what to expect from the study. They will also provide documentation and details about the consent form that the volunteer needs to sign. The following information must be given to each volunteer:
- What the research is and why it’s being done
- How long it will last
- Confirmations that participation is entirely voluntary and that declining participation will not affect the availability of necessary care
- A detailed explanation of all procedures involved in enrolling in the clinical trial
- Potential benefits and risks associated with the research
- Any discomforts (e.g. injections, frequent blood tests)
- Other treatment options, if any
- How your privacy will be protected throughout the trial
- What happens if you’re injured and where to get help
- The participant’s rights, including the right to refuse or withdraw from the trial at any time
Participants should thoroughly review all the information presented during the informed consent process. This will help them understand the risks and safety of the clinical trial. They should also use this opportunity to ask any remaining questions they may have.
Why is informed consent important?
Informed consent is essential in every clinical trial to ensure participants fully understand all aspects of their involvement. It guarantees that participants are aware of the trial’s purpose, procedures, risks, such as possible illness, benefits, and their rights, fostering trust and transparency. This consent process also helps minimise misunderstandings or disruptions, as participants are better prepared and informed.
For research staff, it means smoother trial operations and ethical adherence, as participants who comprehend the clinical trial process are more likely to cooperate and engage responsibly. Informed consent protects both the participants’ well-being and the integrity of the research.
What are the 4 principles of informed consent?
Informed consent is not only about providing general information to help participants understand clinical trials; it also encompasses four fundamental principles. These principles ensure that participants are well-informed, voluntary, and ethically engaged in the research process.
Decision-making capacity
Decision-making capacity is essential for informed consent. This principle ensures that participants have the ability to make informed decisions. Decision-making capacity includes:
- understanding the options available,
- grasping the consequences of each option,
- and, evaluating the personal costs and benefits relative to their values and priorities.
If a participant cannot fulfil these components, a surrogate decision-maker, such as a family member or court-appointed guardian, may step in. Having decision-making capacity doesn’t mean always making decisions that others agree with, but it does mean understanding and explaining the options and their implications.
Disclosure
Disclosure involves providing sufficient information to the participant so they can make an informed decision. This includes:
- explaining the risks and probabilities of each risk,
- detailing the benefits and likelihood of benefits,
- and, answering any questions in clear, understandable language.
Participants do not need every detail but should receive enough information to make an intelligent decision about their involvement in the trial.
Documentation of consent
Documenting consent is crucial, especially for invasive tests or treatments with significant risk. This process typically includes:
- providing a written consent form along with a verbal explanation, preferably in the participant’s native language,
- discussing the medical condition that necessitates the procedure or treatment,
- explaining the purpose, benefits, and potential complications,
- describing alternative treatments and their relative risks and benefits,
- and, discussing the consequences of not undergoing the treatment.
Both the participant and the doctor should sign and date the consent form. Participants should also receive a copy for their records.
Competency
Competency is a legal term indicating that a person can make and be accountable for their decisions.
In the context of informed consent, it ensures that participants have the mental and emotional capacity to understand the trial and make informed decisions. Technically, a court of law can only declare someone “incompetent”.
When is informed consent obtained during a clinical trial?
Informed consent is obtained before the first trial-specific activity is undertaken, including screening procedures. This is documented by an informed consent form (ICF) signed by the participant. This document is kept on file for the duration of the trial, as well as a specified time afterwards for auditing purposes.
However, informed consent is not a one-time event. Throughout the trial, new information may emerge that could affect the participant’s willingness to continue. Therefore, it is essential to maintain open communication between the research staff and participants.
How is informed consent obtained for a clinical trial?
Informed consent for a clinical trial can be obtained through paper or electronic forms. These forms are reviewed by individuals with appropriate scientific training to ensure clarity and completeness.
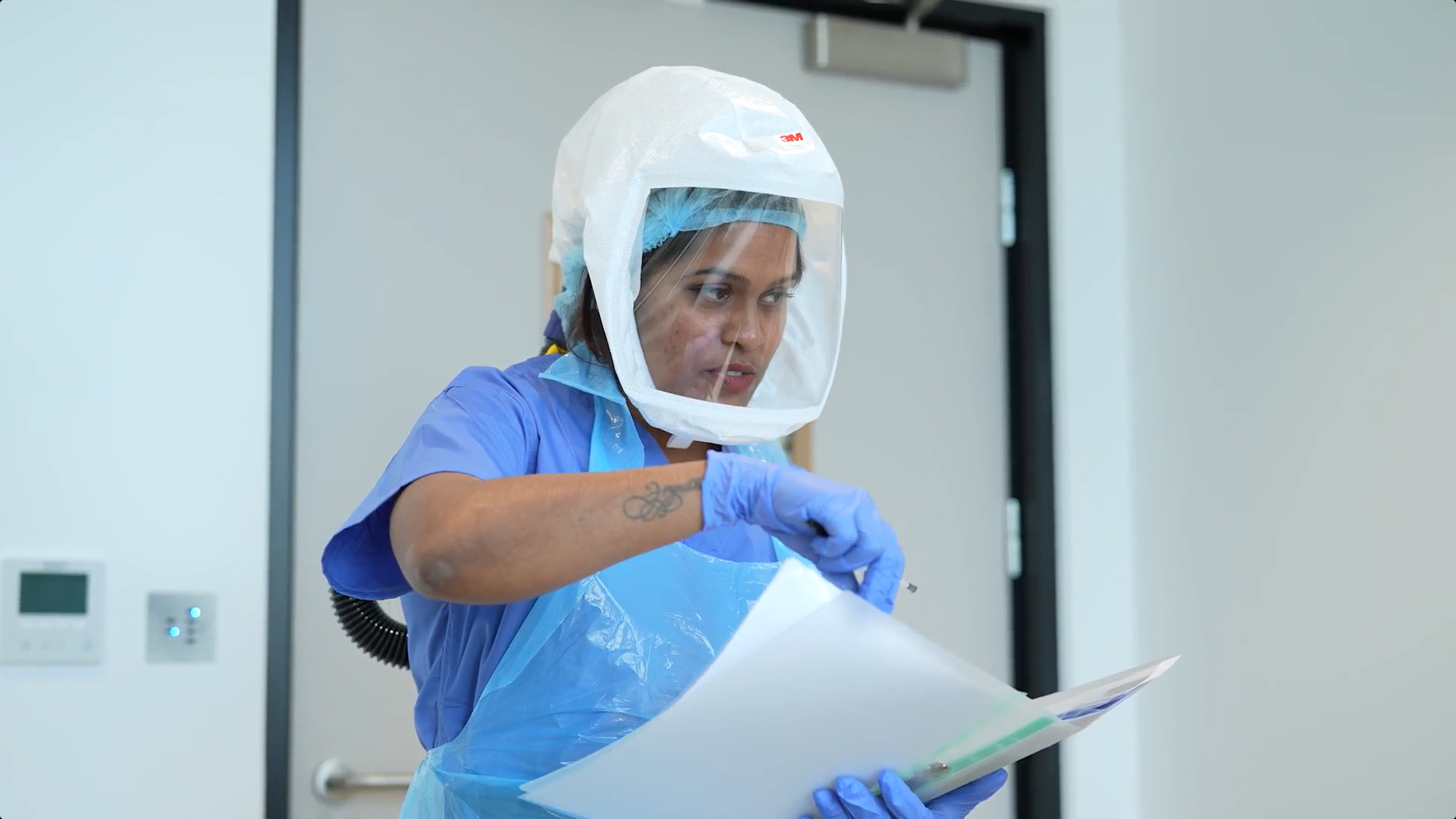
At FluCamp, participants complete paper consent forms in person. This form is thoroughly reviewed with the participant by trained staff, who explain the details and answer any questions.
What next?
We’ve covered the importance of informed consent, the principles that underpin it, the timing and process of obtaining it, and how it is managed at FluCamp. Understanding these elements ensures that participants are well-informed and ethically engaged in clinical trials.
If you’re interested in participating in a clinical trial or have any questions about safety, please visit our trials page or contact us. Our team at FluCamp is ready to provide you with all the information you need to make an informed decision.