During the last 10 years, it has been proven that there could be a connection and repercussion between hydration and different respiratory diseases. Dehydration is a common symptom of allergies but an unusual trigger for asthma.
Index:
- What happens when you are dehydrated or not hydrated enough?
- What is the trigger between dehydration and asthma?
- Does dehydration trigger exercise-induced asthma (EIA)?
- Tips for staying hydrated
So, what happens when you are dehydrated or not hydrated enough?
Between 50-80% of the human body is made up of water, therefore, staying hydrated has a big impact on most of our organs and our health.
Elderly people need to be reminded of drinking enough liquids as they lose the sensation of thirst. Children need more water in their bodies, 65% of their total body weight. In addition, their thirst mechanism is not as developed as in adults.

Source: https://www.bupa.co.uk/health-information/nutrition-diet/keeping-hydrated
What part does histamine play in hydration
Histamine is a natural hormone in the body produced by mast cells, basophils, and other immune cells in several tissues; and it is stored in mast cells that line most tissues inside our bodies.
It is used by the immune system to cause inflammation, helping to trap and kill pathogens, and released during any allergy reaction and asthmatic responses acting as a:
- mediator of inflammation,
- effective neurotransmitter,
- distributor of fluids diverting water away from non-vital areas of the body (such as the skin) and diverting it to vital organs as the lungs
Our lungs need to stay well hydrated to permit efficient gas exchange between a complex inner aqueous body system and a dry outside atmosphere.
The movement of fluid between the airspaces, interstitial, and vascular compartments in the lungs plays an important physiological role in the maintenance of hydration and protection of the lung epithelium and significantly contributes to proper airway clearance.
As a neurotransmitter, It also regulates the flow of water throughout the body guaranteeing all cells stay well hydrated.
According to the last studies from the University of Chicago, when cells recognise that water levels are low, they start to release histamine. When histamine levels are elevated, the brain (hypothalamus) signals the release of ADH (antidiuretic hormone or vasopressin). When the kidney detects ADH it activates a mechanism to put water back/conserve water into the bloodstream, stopping the body from urinating and reducing sweat rate.
Other local functions of histamine:
- to dilate and to make permeable the blood vessels inside the lungs guaranteeing that they have enough hydration, so blood flow slows down and some of the fluid in these vessels leaks into the spaces between the cells, causing inflammation of the airways and them narrower than normal
- to increase mucus production and to smooth muscles wrapped around the airways to tighten and contract, causing the main symptoms of asthma – shortness of breath, tightness in the chest, increased sputum production and wheezing.
Does dehydration trigger exercise-induced asthma (EIA)?
Assuming that the nose is the mechanism responsible for humidifying inhaled air to body temperature, it is logical to think that vigorous activity (e.g. running or doing cardio), makes you breathe so fast that your nose can’t keep up the rhythm of your breathing causing dehydration. Since we breathe through our mouths while running or doing intense exercise, this causes the cells in the airways to give up some of their moisture to humidify the inspired air, giving, as a result, localised dehydration of the airways.
This mechanism is aggravated when the inhaled air is cold – which tends to retain less water – making the cells in the airways work overtime to humidify the inhaled air. In addition, cold air needs to be warmed, and airway cells must also give up some of their heat. Therefore, cold air can further dehydrate the airways.
How much should we drink?
Recommendation for keeping your body hydrated, aim for a fluid intake of about:
- 3 L (12 cups) for men (19 years or older each day)
- 2.2 L (9 cups) for women (19 years and older each day)
Quick tips for better hydration
High temperatures during summer and heating during winter increase your chances of becoming dehydrated.
Start and finish your day drinking. Drink regularly – even before you feel thirsty
- Carry water with you throughout the day while at your desk/working from home/outdoors
Drink before, during and after exercising.
Choose to drink mainly water – soft drinks should be consumed in moderation, whether carbonated or not, and sweetened with sugar or fructose are not fluids that should be consumed daily to ensure hydration.
- Drinks and food beneficial for asthma symptoms that may reduce airway constriction and have anti-inflammatory effects on the airways:
- – caffeinated drinks, fortified milk, and water
- – increase your intake fish oil, fruits, vegetables and food high in vitamins D and E
Drinks that might worse asthma symptoms:
- sugary drinks and alcohol
- fast food and meat
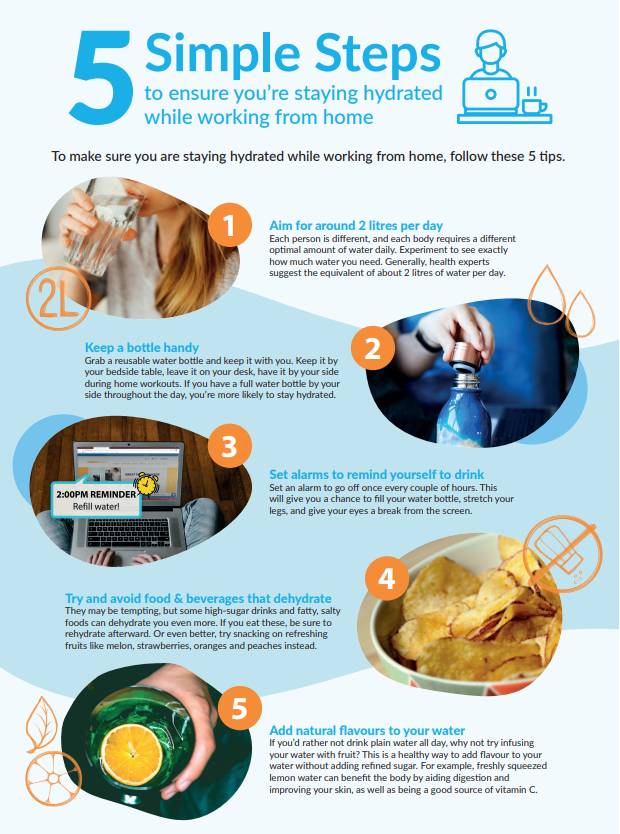
Source: https://hydrate.direct/5-ways-to-stay-hydrated-while-working-from-home
References:
- Kalhoff, H. 2003. Mild dehydration: A risk factor of broncho-pulmonary disorders? European journal of clinical nutrition 57, (12): S81-7
- Gabriel SE & Boucher RC (1997): Ion channels. In The Lung. Scientific Foundations. 2nd Edition, eds. RG Crystal, JB West, pp 305–318. Philadelphia: Lippincott-Raven Publishers.
- PC Potter, M Klein and E G Weinberg: Hydration in severe acute asthma. Arch Dis Child. 1991 Feb; 66(2): 216–219. doi: 10.1136/adc.66.2.216. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1792828/
- Kwi-Baek Kim and Yi-Sub Kwak: Dehydration affects exercise-induced asthma and anaphylaxis. J Exerc Rehabil. 2019 Oct; 15(5): 647–650. Published online 2021 Oct 28. doi: 10.12965/jer.1938470.235. PMCID: PMC6834710. PMID: 31723551. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6834710/
- Manz, Friedrich, and Andreas Wentz. 2005. The importance of good hydration for the prevention of chronic diseases. Nutrition reviews 63, (6) (06): S2-5, http://libproxy.uwinnipeg.ca/login? (accessed in 15 Aug 22)
- Moloney E, O’Sullivan S, Hogan T, Poulter LW, Burke CM. Airway dehydration: a therapeutic target in asthma? Chest. 2002;121:1806-1811.
- Guidelines for staying hydrated communication. Dietitians Canada https://www.dietitians.ca/getattachment/becace49-3bad-4754-ac94-f31c3f04fed0/FACTSHEET-Guidelines-staying-hydrated.pdf.aspx (accessed in 1 Sep 22)
- Simpson AJ, Romer LM, Kippelen P. Exercise-induced dehydration alters pulmonary function but does not modify airway responsiveness to dry air in athletes with mild asthma. J Appl Physiol (1985) 2017;122:1329–1335.
- PC Potter, M Klein and E G Weinberg: Hydration in severe acute asthma. Arch Dis Child. 1991 Feb; 66(2): 216–219. doi: 10.1136/adc.66.2.216. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1792828/ (accessed on 25 Aug 22)
- Al-Zalabani, A. H., et al. (2019). Association between soft drinks consumption and asthma: A systematic review and meta-analysis. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6797295/
- Asthma and alcohol. (2020). https://www.asthma.org.uk/advice/triggers/alcohol/
- Berentzen, N. E., et al. (2015). Associations of sugar-containing beverages with asthma prevalence in 11-year-old children: The PIAMA birth cohort [Abstract]. https://pubmed.ncbi.nlm.nih.gov/25117998/
- Guilleminault, L., et al. (2017). Diet and asthma: Is it time to adapt our message? https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5707699/