Many people are curious about how clinical trials get approval. There’s a strict process, as regulatory bodies need to understand the safety of the interventions that the study will look at. These authorities are involved not only in the approval of the trial, but also consider data collected throughout the study period to determine if the new drug will get approval to become available to the public. In this article, we explore the approval process and look at who is involved.
How are clinical trials planned?
The first step of a clinical trial is a thorough planning process. During this step, the researchers create a complete outline of the study and develop the protocol. These documents contain information about what questions the trial will essentially explore and answer, while also providing more details related to the objectives and goals.
The planning process involves determining how many participants are needed in the trial, as well as how they will be selected. In a Phase 1 trial, for example, the researchers will only require a few people to get a baseline on the safety of a new drug and to start determining the appropriate dosage. In later phases, the researchers will consider a larger pool of participants, especially if the new treatment needs to be compared to a placebo or the current interventions.
During planning, the researchers must also consider ethical factors and decide how the informed consent documentation will be compiled.
Who regulates clinical trials in the UK?
There are two important bodies involved in regulating clinical trials in the UK. The first is the Medicines and Healthcare Products Regulatory Agency (MHRA), which oversees the approval of clinical trials and ensures the safety of participants. The MHRA is also involved in ensuring that trials are planned and designed according to the high standards and compliance requirements it has set.
The Health Research Authority also plays a role in the process. This body takes into account ethical considerations. It helps researchers understand how ethics should be incorporated into a study, with a focus on topics such as informed consent.
There are also independent research ethics committees that review the planning of clinical trials. Before trials can conduct experiments on humans, these committees, along with the other regulatory bodies, must give their approval.
How do clinical trials get approved?
The approval process for a clinical trial involves several rigorous steps. This is because the safety of the study is a critical factor. Apart from safety, there are also processes that will consider ethical elements, as well as efficacy. In this section, we break down the steps involved in the clinical trials approval process to ensure that participants are safeguarded and reliable results are produced.
Peer review
The process starts with a peer review. This involves a group of people who will review all the details from the protocol the researchers developed during the planning process. The group consists of various healthcare professionals, such as doctors. Non-medical individuals also form part of the group. The idea is to ensure that the study’s outline and protocols are properly developed from a scientific aspect, and to identify any potential issues with the trial before it’s allowed to go through other processes, such as funding.
Ethical approval
The next step is ethical approval. This is done by another group. A minimum of one-third of the ethical review team are not in the medical industry and have no background in clinical research. The Health Research Authority of the UK organises the creation of the Research Ethics Committee, which looks at the risks, benefits, qualifications of the research team, how participants will be recruited, and the trial’s goals. The REC can demand changes before approval and clinical trials must notify the committee of any protocol amendments or serious side effects during the trial.
Other checks
Some clinical trials will need to go through more checks and approval processes. This is usually the case when there are additional factors to take into consideration. An example would be a trial that will expose the participants to radiation. A specialist committee with experts on the specific topic will be required to run additional checks on the protocols to ensure that they follow regulatory standards.
Trial authorisation
After these checks and processes, the researchers must submit all of the content to the MHRA. This body will then review all of the data and decide if it will issue a Clinical Trial Authorisation for the study.
Trial authorisation also requires an investigational medical product dossier and a covering letter. A manufacturer’s authorisation and a copy of the labels used on the investigational medicinal products are also needed in most cases.
What are the key phases of clinical trials?
There are four main phases that form part of a clinical trial. During Phase 1, the purpose is mainly to determine the safety of the intervention, and also to decide the most appropriate dosage. In Phase 2, the trial is done on participants with the condition to determine the effectiveness of the drug or intervention.
Phase 3 usually divides participants into groups, which allows researchers to compare the effects of the new drug to the efficacy offered by existing treatment options or sometimes a placebo. After the drug is approved by the MHRA, Phase 4 clinical trials continue to collect data on the longer-term effects.
How are clinical trial results evaluated?
Once the clinical trial starts, results are consistently collected and evaluated. This is an important part of the trial, as it allows the regulatory bodies and those involved with monitoring the study to determine the efficacy of the new intervention. The data is statistically analysed against existing treatment or base results, depending on what the trial is testing, to determine the effectiveness of the treatment. It also enables these authorities to identify any potential risks or side effects, in which case appropriate steps can be taken.
The evaluation process also allows the results of the clinical trial to be organised and then published in scientific journals. A peer review process can also help to provide unbiased approval for the data. All of this allows researchers, patients, and healthcare providers to get a better idea about the efficacy of these treatments, while also understanding the safety profiles.
What happens after a clinical trial is approved?
At the end of the clinical trial period, all of the data is compiled, and reports are created. These documents, along with other supporting information, are sent to the regulatory bodies for approval. If the drug gets approval, it becomes available to the public. The organisations involved with the intervention continue to monitor the effects through longer-term studies. This helps ensure that they get a better idea of how the treatment affects people outside of the clinical trial environment.
Regulatory bodies may also use data collected after the clinical trial to create appropriate restrictions in terms of how the drug can be marketed and prescribed to patients.
How can participants get involved in clinical trials?
Now that you have a better understanding of how clinical trials get approval, you may have questions about participating in these studies. Every participant of a clinical trial plays an important role in helping push the medical industry forward and bring more effective treatments to the public.
Start by learning about the things you need to know before you participate in a clinical trial. Once you feel ready, you can search for clinical trials that you are eligible for and contact the organisations involved.
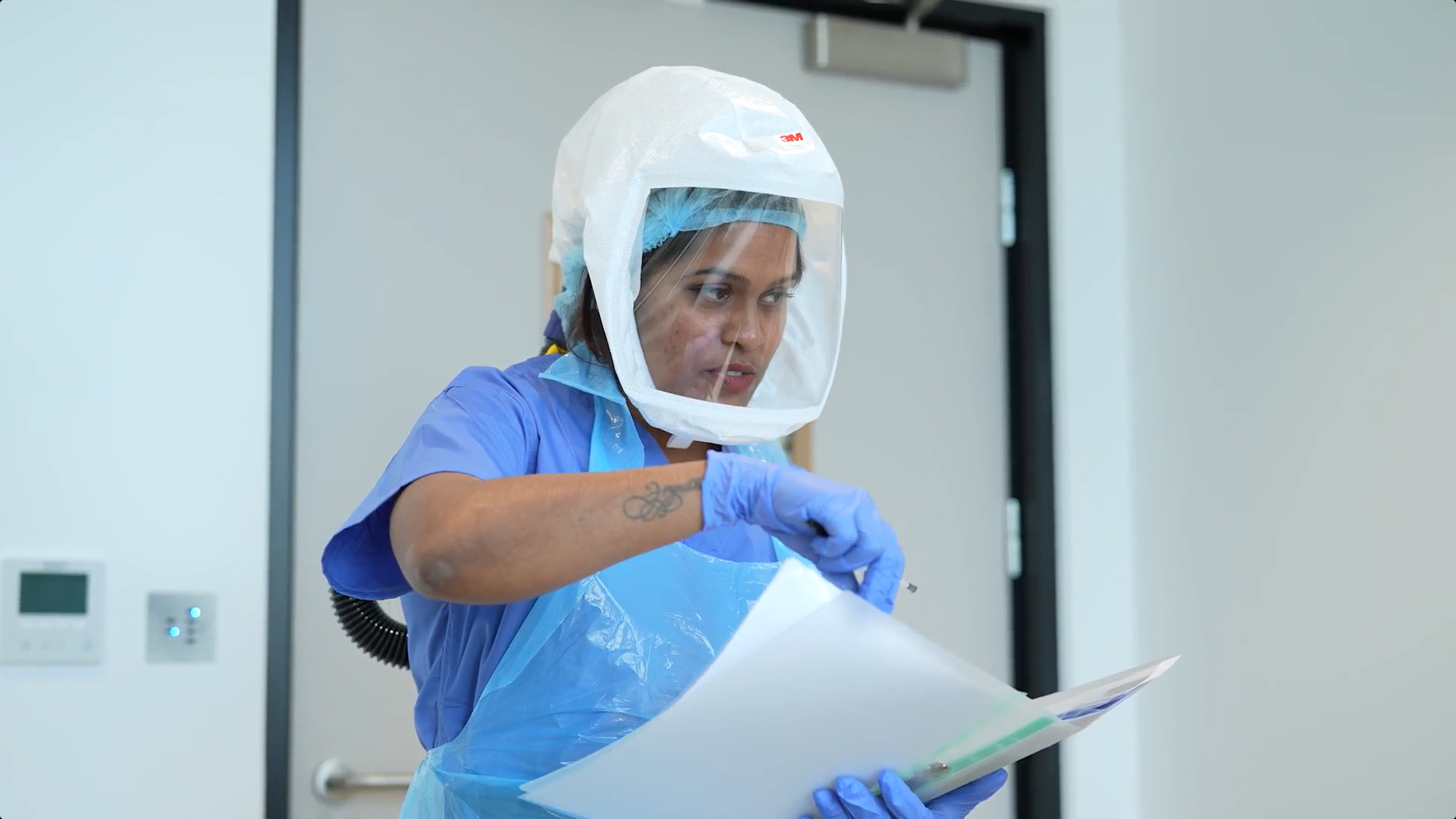
Before you can start your engagement in these trials, you first need to give informed consent. This plays an important role in the process, as it ensures you know exactly what you sign up for. The informed consent will provide comprehensive details about the study and the interventions that they are testing. Once signed, you’ll be provided a private room with a residential program. If the clinical trial is not residential, you’ll need to report to the facility on a regular basis.
What next?
Approval for clinical trials goes through a thorough process that involves peer reviews, ethical approvals and sometimes additional checks. Learning more about the clinical trials approval process allows you to see just how strict regulatory bodies are to ensure patient safety. FluCamp offers a safe environment where participants are given their own private rooms. To find out if you are eligible for one of FluCamp’s clinical trials, fill out the contact form and you’ll be sent details about upcoming studies.